It can feel pretty scary to consider your organs might be falling out, especially if you don’t know why it’s happening or how to fix pelvic organ prolapse. Let me share a little story about prolapse and what I know now that will hopefully give you peace of mind.
Years ago, before I became a pelvic physical therapist, I had met up for drinks with a friend. After a few glasses of wine, she confided in me that her uterus was falling out of her vagina. At first, I thought she was joking or at least exaggerating. She always had a flair for the dramatic, especially after a few chardonnays.
At the time, I honestly couldn’t grasp what she was talking about. How on earth could this be happening to my seemingly healthy friend? She was in her 40s, a bodybuilder, and seemed to be pretty healthy. I mean, she had given birth a few times, but it was hard for me to imagine that this kind of thing could happen to her. She was really concerned that she would need to have surgery to put her organs back in place. Yikes! I was speechless.
Fast forward many years, I understand things on a much deeper level now. I’ve been working with and treating so many women with prolapse. Let me assure you that it’s not usually as dire or scary as it sounds. It’s totally treatable.
What is Pelvic Organ Prolapse (POP)?
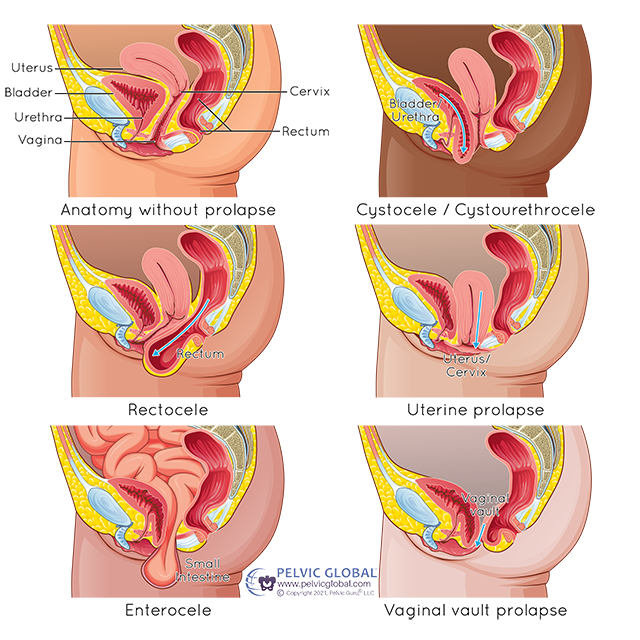
Basically, it is when one or more than one of your pelvic organs (bladder, uterus, urethra, rectum, small intestines) bulges, protrudes into or slips into the vagina. The top of the vagina can also collapse on itself and enter the vaginal canal. *You can note the different types of prolapse in the photo above.
There are varying degrees or stages of prolapse, which measure the severity of the situation. It is thought that around 50% of women at some point will have some degree of POP. So, it’s no surprise that I often feel a slight prolapse in my patients during internal pelvic sessions. Sometimes they aren’t even aware they have it. Within a few sessions, it usually resolves. Given the stats, this sort of mild prolapse is fairly common, easily treated, and nothing to worry about.
What are the Signs and Symptoms of Pelvic Organ Prolapse
The biggest report I hear is the feeling of heaviness and pressure in the pelvic area, below are a list of the most common symptoms.
- A feeling of heaviness or pressure in the pelvic floor, the vagina.
- Feeling like a golf ball, tennis ball, or a sense of having a tampon stuck in the vagina.
- Bladder symptoms are common including loss of control or not being able to empty completely.
- There may be pain with penetration.
- Back pain
- Some report a feeling of looseness, weakness, or a sense of something slipping down.
- Sometimes patients report seeing something peeking out of the vagina when looking at its entrance.
- Constipation issues can occur with rectal prolapse (rectocele).
When the rectum is bulging into the vagina, patients sometimes need to splint the vagina – push a finger into it to assist the stool to pass through the rectum.
Causes of Prolapse and The Misconceptions
Now if you’ve been researching POP and its causes, you might be under the impression that it’s all because of weakness in the pelvic floor muscles. That’s really only part of it and not the whole story! Don’t order those Kegel weights until you hear me out.
Pelvic muscle weakness is only one piece of the puzzle, in fact, believe it or not, many of my patients with prolapse have sufficiently strong pelvic muscles. Often they have very tense pelvic muscles that need to be released before strengthening them. Trying to strengthen dysfunctional muscles can complicate progress.
Organs Under Pressure
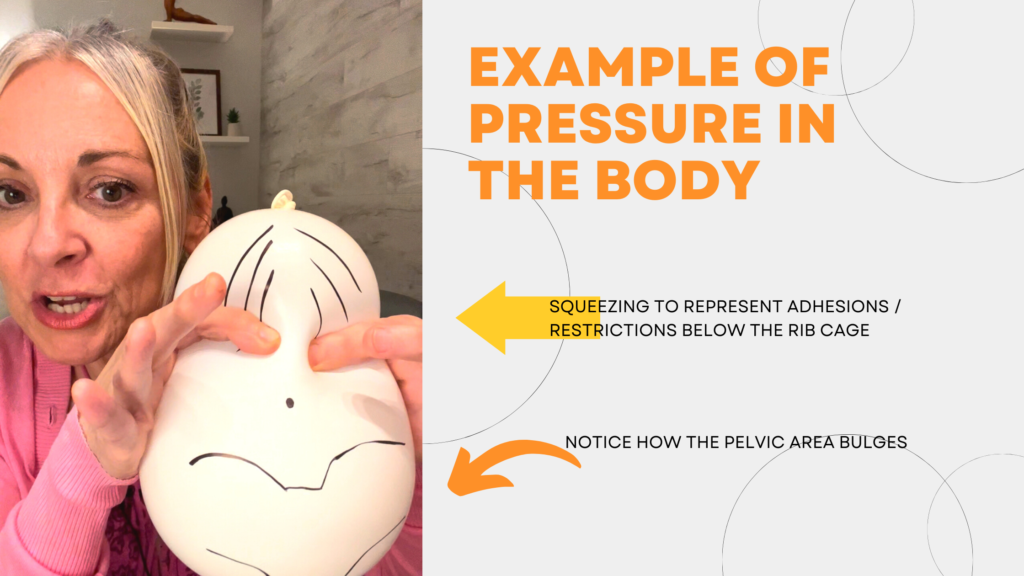
Prolapse, hernias, and diastasis recti are all examples of herniation. Herniation occurs because tissues in the body can no longer handle the pressure placed upon them. There are several things that contribute to losing the ability to handle the pressure system of our body cavities.
Our Boney and Soft Tissue Framework
The function and integrity of the pelvic organ support system are dependent on the bony frame of our skeleton and connective tissue. This includes the ligaments of the uterus, the suspensory ligaments of the bladder, the diaphragm, and the muscles and fascia above and below the pelvic floor. It’s all connected!
Posture/Alignment Habits
The way we carry our bodies; postural habits can predispose us to not being able to handle the pressures placed upon our bodies. See, when we have a neutral, symmetrical alignment, the muscles and organs are positioned optimally to respond to the forces of gravity we experience on a regular basis. Postural imbalances can affect the integrity of the soft tissues, muscle control in the core and pelvis, and ultimately the ability to handle intra-abdominal pressure.
Changes to the Fascia
Our fascial system is a three-dimensional web of connective tissue that provides both support and mobility to our entire body. Fascia has a strong yet fluid quality to it. When it is injured or scarred, it can become thick and dry, exerting massive pressure on the tissues near and far.
Scarring / Adhesions
Adhesions from pelvic and other Injuries, childbirth, traumas, infections, and surgeries can alter the quality of the fascia in the body as described above. The restrictions can glue one organ on the other (ie, the uterus to the bladder) which adds weight and pressure to the pelvis. All kinds of surgeries can contribute to scar tissue, and lead to prolapse. Hysterectomy can further complicate prolapse since important suspensory ligaments that provide support to the pelvic floor and its contents are also removed.
Hormones
Hormonal changes that occur during perimenopause and menopause can cause the connective tissue of the vagina to become thinner, less springy, and less resilient.
All of this pushing and pulling on the soft tissues and organs can create more asymmetry, weaken tissues and alter the ability to handle the pressure system of the body and cause herniation or prolapse. It’s important to understand how improving postural alignment and restoring the dry, restricted soft tissues to a more fluid, springy state is as important as strengthening muscles when it comes to fixing pelvic organ prolapse.
What To Do If You Suspect Prolapse
My first suggestion is to find a pelvic physical therapist who has experience treating this. Choose someone who understands that there is more to it than fitting you with a pessary or prescribing Kegels. (A pessary is something that sort of looks like a contraceptive diaphragm that is fitted and placed vaginally to support the structures. If it’s necessary to have one, my hope is that it’s temporary until the neuromuscular system adapts to the training).
If you have abdominal or pelvic adhesions/restrictions, you’ll need manual therapy to help release them. This will help the fascia return to its hydrated, springy, resilient state. I suggest working with a PT who understands the complexity of prolapse. Make sure you ask questions before committing. It also may be a good idea to get help with hormonal balance and diet through a nutritionist, naturopath, or acupuncturist.
Below are some other things to consider working on if you have or suspect prolapse.
We Are Dynamic Creatures
We are dynamic moving targets. I’ve tested my patients internally while lying down and in standing to assess how things change in different positions. When they are standing, the pressure changes and gravity is working against them, so the prolapse can worsen. This can vary from day to day depending on where they are in their cycle, what’s going on with their stress level, and how tense they are in their shoulders and rib cage. This is why I don’t really focus too much on what degree of prolapse my patients have. It’s more important to me that we monitor symptoms, strength, mobility, and the ability to handle our day-to-day functional activities.
Resilience is Important
Having a supple, resilient, and relaxed pelvic floor is important. This happens when we release stuck tissues that are inhibiting the ability to create a dynamic response to stressors. The stressors like sneezing, coughing, lifting, running, and jumping, increase intra-abdominal pressure.
The muscles of the pelvic floor and core, the diaphragm, and rib cage need to be able to expand or contract on demand to this load or extra pressure without thinking about it first. This requires regular movement, mobility, practice, awareness, and training.
A Mindbody Approach
Of course, what you eat, drink, or don’t eat or drink can affect the tissues of your body, so doing your best to eat clean, avoid inflammation, sugar, alcohol, and staying hydrated are important. Having a resilient nervous system, and being able to calm your mind affects your tissues as well. If you’re constantly going going going and don’t take time to integrate mind and body, breathe and become present, that will affect your outcome.
Will the FeminEnergy® Program help me if I have Pelvic Organ Prolapse?
The short answer is YES!
All of the things I’ve mentioned above are big parts of the Program; from learning the feminine alignment to mobilizing fascia, breath work, strengthening, a resilience mindset, and calming the nervous system. We work from the ground up, from the inside out to create an atmosphere of healing. I’m with you every step of the way and there to answer your questions. The things we work on in the Program will give you the tools you need to handle the pressures (physical and emotional) that we deal with.
Depending on your level of severity, you may need to have some manual treatment as well. You can try working with someone in your local area, and if you can’t find someone, I do offer intensive treatment sessions for out-of-town patients. If that’s your situation, please feel free to set up a Discovery Visit with me and we can customize a plan for you.
I have physically felt, with my hands, the dramatic shift and lift in the placement of the pelvic organs when my patients assume the feminine alignment from my program.
So, It’s my hope that I’ve enlightened you about how to fix pelvic organ prolapse. If you are experiencing symptoms, I hope I gave you a little peace of mind. Everyone’s journey and timeframe with this is unique, some require more work than others. Have patience and give yourself grace. Sometimes people require surgery, but I believe that to be a small percentage.
How About My Friend?
Now that I know what I know, it’s not so hard for me to believe that she had prolapsed. She had given birth twice and had some surgeries, I knew that she had some gastrointestinal issues, and she was a bodybuilder.
All of this had predisposed her to scar tissue and uneven pressures. Her bodybuilding routine included strenuous, heavy lifting and I would be willing to bet that although she had ripped, washboard abs, she had not learned how to properly activate her core/pelvic floor and diaphragm together, I see this all the time with athletes.
She likely was bulging rather than lifting her pelvic floor when she was doing her clean and jerks. She got the help she needed and no surgery was necessary.
Prolapse photo used with permission from Pelvic Guru® LLC www.pelvicglobal.com